Many individuals suffering from addiction experience stigma associated with their disease. Stigma also exists within the culture of addiction treatment and community recovery support groups.
In this story, stigma related to medication support in recovery illustrates how contempt prior to investigation can be fatal and yields unhealthy exclusivity to a rich recovery cultural heritage. (Names and ages have been changed to protect identities)
Meredith was a 24 year old woman who first tried opioids at the age of 15. She was a cheerleader, an A student and an athlete when a friend brought pills over to the house. Meredith couldn’t forget the feeling the first time she tried opioids. This drug helped her manage feelings of anxiety and negative body image. This drug made her numb to the feelings of anger relating to her parent’s divorce. Over the next four years she performed in school but opioids slowly became the centerpiece of Meredith’s life. After high school graduation, she began smoking heroin because it was cheaper to maintain a daily habit and within six months she was injecting. She went to “rehab” twice, expensive programs with false promises of 80% long-term success rates. She dropped out of community college, she drifted between her parents, drug houses and worked at strip clubs. Coming and going with different people, things began to go missing and she became unwelcome at home with family and friends.
Meredith went to detox a few times, participated in outpatient treatment groups, and went to meetings, but always there was heroin. Her body and brain had changed with the physical dependency that demanded use every 4-6 hours or face traumatic withdrawals. She accepted that life had become unmanageable. She entered a third rehabilitation program that offered her choices to support her recovery. Meredith chose to stabilize on Suboxone (buprenorphine/naloxone) as she entered a residential treatment program.
She trusted the counselors around her, and her peers. She also felt physically and emotionally well for the first time she could remember. She developed bonds in the treatment and recovery community, but often felt like an outsider. “You really should get off that stuff.”
“You know you aren’t really clean.” That message from a person in the recovery community grabbed hold. Meredith had always felt like an outsider, to her friends on the cheerleading squad and even to her own family. She desired acceptance and would risk her life to achieve it.
Meredith succeeded in completing her residential program, she transitioned to an outpatient program with a drug-free home to live in. She worked with her doctor to take less medication. One day at a community fellowship meeting she was told, “Don’t come back until you are really clean.” She was again unwelcome. Devastated, she chose to comply with the demand. She stopped her medication without telling her doctor, she isolated and two weeks later found heroin again. Meredith overdosed and passed away the first time she returned to heroin after being clean for 7 months.
Meredith’s death was preventable. As a physician who has helped patients manage their disease of addiction for more than 15 years, it is clear that Meredith for the first time was succeeding in her recovery. The disease that had made her unwelcome in her family had been effectively treated for the first time. She was a victim of a culture of recovery that continues to be challenged to accept the scientific best-practices for managing this disease. Meredith had become unwelcome among her cohort of people in recovery for choosing to manage her disease with medication support. She was stigmatized within a culture of people in recovery.
Stigma is defined as: An attribute, behavior or condition that is socially discrediting. Known to decrease treatment seeking behaviors in individuals with substance use disorders. (Recovery Research Institute 2017)
Those who suffer from substance use disorders experience stigma on many levels. Societal stigma surrounding this disease has been shown to prolong the illness and results in people seeking treatment later than they otherwise might due to fear of discovery, due to fear of judgement by others. In many countries strict patient confidentiality laws protect the identity of individuals in an attempt to help prospective patients feel safer. However, within the drug and alcohol treatment field change that benefits patients pursuant to the general body of scientific evidence regarding best-practices has continued to be slow. Out in the rooms, a mixed-bag of old culture and new culture has also been challenged to embrace the required sea-change to save more lives from the terrible opioid epidemic afflicting America.
Thankfully, through the voices of patients in successful recovery and the leadership of individuals within the addiction treatment field, science is empowering more patients to achieve success. Patients have expanding access to individualized treatment plans. Patients and families are empowered to ask questions informed by the scientific data. The best practices represent clinical research informed by leaders in this field from an international scope as this disease is unfortunately ubiquitous to the human condition.
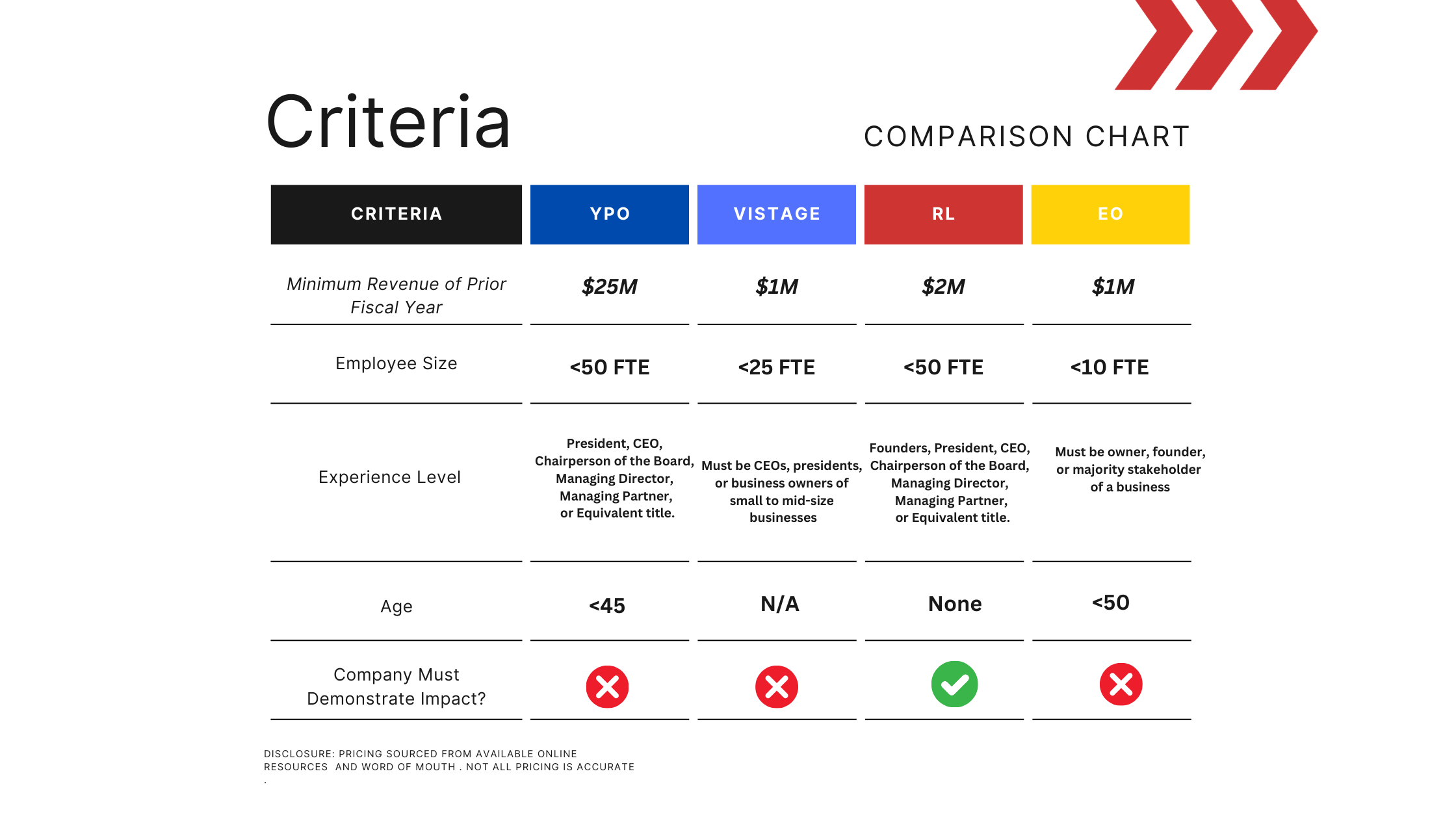
A compelling study by R.E. Clark et. al. from 2015 illustrates the prevalence of relapse and the total cost of care among Medicaid patients with opioid use disorder treated with behavioral-health interventions only, or treated with medication support. Inspection of the results reveal a 50% probability month-over-month in the probability of opioid relapse compared to roughly 5-6% for patients receiving medication support. In short, medication support conferred ten times the likelihood of remaining abstinent from opioids beginning in the first month of treatment. The treatment effect remains comparable over much of the next 36 months in this cohort study. All patients deserve access to the path which offers the greatest potential for success.
Patient choice and a diversity of treatment options leading to an improvement in access to individualized care represents the future of addiction treatment. Inclusivity as opposed to exclusivity in treatment centers and fellowship groups recognizing that everyone who works within this field desires the same outcome for their patients, success in long-term recovery. Freedom to recover without stigma associated with how a person chooses to recover.
In America, I am grateful to see policy makers, insurance companies and clinical programs working together to help more patients achieve success in their recovery from substance use disorders. This is Real leadership in the face of the opioid epidemic.